Bridging the Gap Between the Science & People Affected by Traumatic Brain Injury
Author: Angelica Sotelo || Scientific Reviewer: Jude Baffoe-Bonnie || Lay Reviewer: Aarohi Shah || General Editor: Erin Michel || Artist: Matthew Jozwik || Graduate Scientific Reviewer: Carolina Cabán Rivera
Publication Date: May 10, 2021
Introduction
Most Americans have probably seen media coverage of a National Football League (NFL) game. Because American football is a full contact sport, it is probably not surprising that frequent collisions between players result in concussions, or “mild” traumatic brain injury (TBI) [1]. While concussions have been associated with American football and its players since 1994, athletes are not the only people affected by them [2]. 69 million individuals sustain TBI each year worldwide [3]. According to the Centers for Disease Control and Prevention (CDC), while a concussion itself is not life-threatening, it is the after effects of the concussion that contribute to complications which may hinder a person’s quality of life for some time [1]. Recent research on the oculomotor system and neuro-optometric rehabilitation may offer affected individuals more opportunities for concussion recovery. Concussions affect our brain in a multitude of ways, including our physical, chemical, mental, and visual processes; however, neuro-optometric rehabilitation is a glimmer of hope for those recovering from traumatic brain injury.
Defining Concussions as “Mild” Traumatic Brain Injury
Establishing that the damage begins in the brain is the first step in understanding how concussions affect our brain’s various processes. The brain itself is encased by the cranium, a bony structure which helps protect the brain from injury [4]. The skull is the combination of the cranium and other bones that protect the brain. In between the skull and the brain are the meninges: three layers of tissue that serve to protect the brain and spinal cord [4]. Even though the brain has all of these protective mechanisms, damage is still possible.
A concussion is a mild form of TBI, which can be caused by a hit to the head (a bump, blow, or jolt) or by a hit to the body [1]. When this sudden impact occurs, it causes the brain to move inside the skull. As stated by the CDC’s “Heads Up” initiative, this results in various chemical changes in the brain as well as brain cells potentially being damaged and stretched [1]. Any type of TBI affects a person’s quality of life in the short term and/or long-term [5]. The four main areas affected by concussions are thinking, sensation, language, and emotion [5]. The CDC details the effects of concussions as a variety of symptoms within each area. These symptoms are some of the many examples that show how concussions affect the physical, chemical, mental, and visual processes of our brain. Some symptoms in each of the four categories include [5,6]:
The greater the force of the impact, the more severe the concussion symptoms [7]. After sustaining one concussion, a person is much more likely to suffer from a second one. Moreover, a second concussion tends to cause symptoms that last longer [7]. The signs and symptoms of TBI may be overlooked by many people, even the individual affected. It can take days or even months for symptoms to be noticed [5]. This is because people who are suffering from TBI can appear unaffected on the outside. Sometimes, the person may not be able to recognize or want to admit that they are struggling [5]. When an individual’s physical, chemical, mental, and visual processes are altered from a concussion, it can be difficult to reason through what is happening, let alone express to someone clearly what it feels like. However, studies on the oculomotor system have been instrumental in understanding and treating the far-reaching effects of TBI.
How Head Impacts like Concussions affect the Oculomotor System
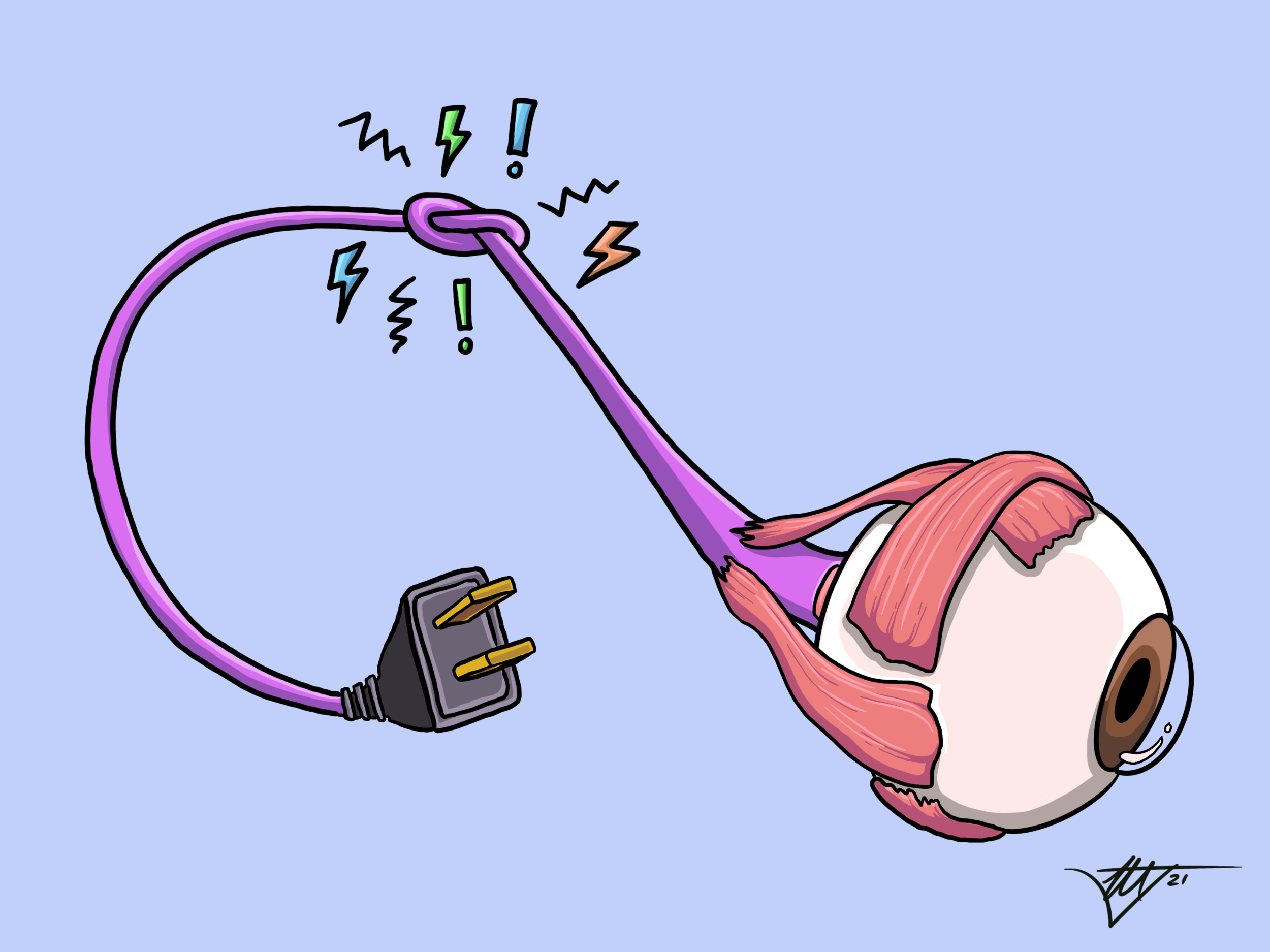
The oculomotor system is how our brain processes information through our eye movements. In fact, more than 70% of our brain is dedicated to vision, and our eyes receive 80% of all the sensory information we take in from the world [8]. Because our brain is so involved in how our eyes function and process information, our eyes can be impaired as well when a concussion occurs. 90% of patients with TBI experience visual symptoms as a result of the close relationship between our brain and eyes [8].
One such visual symptom is convergence insufficiency [9]. Convergence is a form of vergence that describes how the eyes turn inwards towards the nose in order to look at an object. Convergence insufficiency describes the opposite. It is a phenomena where the eyes have difficulty working together and focusing on an object. Instead of both eyes turning inwards, one eye turns outwards. This can result in symptoms such as blurred vision, diplopia (double vision), and headaches [9]. When these symptoms are present, a person’s depth perception can be affected. Good depth perception allows us to track objects in front of us as well as do near sighted activities such as reading and writing [10]. However, when an individual is experiencing convergence insufficiency, their ability to track objects and do near sighted tasks may be limited [10]. These symptoms may be present immediately after the head impact occurred or they may develop days after the injury [5]. Various studies have explored how long convergence insufficiency affects the individual after they have sustained a concussion.
Using Soccer as a baseline for studying the visual effects of a concussion
A 2016 study by Dr. Kawata from Temple University’s Kinesiology Department had 20 healthy volunteers participate in a soccer heading exercise followed by the near point of convergence (NPC) assessment [9]. A soccer header is a technique that is used to control the ball by using the head to pass or shoot. This technique was used to give the volunteers mild head impacts. The NPC assessment is a way to determine how the mild head impacts affected the individual’s oculomotor system. The NPC is the distance where both eyes can focus on an object before experiencing the symptoms of convergence insufficiency [9].
These volunteers were split up into two groups- a soccer heading group (n=10) and a control group (n=10) [9]. A JUGS machine (an automated throwing machine) was used to propel the soccer ball up to speeds of 11.2 m/s (25 mph) towards the subject who was 12 m (40 ft) away. Once the soccer ball reached the subjects, those in the soccer heading group were asked to perform 10 standing headers with a one minute break in between each one. In contrast, those in the control group had to remain standing and inactive for 10 minutes [9].
After the soccer headers were completed, both the soccer heading and control groups completed the NPC assessment [9]. For the NPC assessment, the subjects were seated with their head upright, directly facing a Snellen chart. A Snellen chart is an eye chart used to measure visual acuity, which indicates how sharp or clear a person’s vision is [11,12]. Reading the letters on this chart is a common test used during check up appointments in primary eye care visits [11]. The subject was asked to focus on a single letter as the chart was moved along the length of a ruler, towards them at a rate of around 1-2 cm/s [9]. When the subject verbally told the tester they were experiencing diplopia (double vision), and could no longer see the chart as a single object, the NPC measurement was taken in centimeters as the distance between the subject and the Snellen chart. The NPC assessment was done at pre-, 0 hours post-, and 24 hours-post-heading [9].
The results of the NPC assessment demonstrated the negative effects repeated head impact can have on the oculomotor system by revealing convergence insufficiency [9]. At 0 hours post-heading, the NPC was 3 cm; and it increased to 3.65 cm at 24 hours-post-heading [9]. The increase from 3 cm to 3.65 cm is an indication of convergence insufficiency because the Snellen chart had to be kept farther away for the participant to be able to focus on it after post-heading. Another way to think about this is that the closer the Snellen chart can get, the less affected the oculomotor system of said participant is. The results suggest that convergence insufficiency is still present 24 hours-post-heading.
Dr. Kawata’s study references a 2014 study by Dr. Mucha from University of Pittsburgh Medical Center, which provided more insight into the persistent nature of convergence insufficiency [13]. Dr. Mucha used the NPC assessment and observed athletes approximately 5.5 days post concussion. The resulting average NPC was 4 cm greater than the control group. At approximately 5.5 days-post-heading, convergence insufficiency was still seen as evidenced by blurred vision and diplopia. Dr. Kawata’s study acknowledges that it can be difficult to compare NPC scores across different studies given they all use different levels of head impact severity [13]. However, the data from both Dr. Kawata’s study and Dr. Mucha’s study show evidence that convergence can be significantly affected and present as convergence insufficiency by even the smallest magnitude of head impact for more than 24 hours [9,13].
When blurred vision and diplopia occur in an isolated incident, it might not be apparent how disorienting it can be to live with these recurring symptoms for multiple days on end. The ability of our eyes to work together is instrumental in how we function in the world around us. Our eyes have to be able to see a singular object in front of us and maintain that object in focus for an extended period of time. This is an innate process that we are not necessarily conscious of, yet it is a key task that the brain and oculomotor system execute together on a daily basis. During concussion recovery, it is possible to re-establish a strong connection between the brain and the oculomotor system through neuro-optometric rehabilitation.
Neuro-optometric rehabilitation as a Treatment Option for Traumatic Brain Injury
Concussions affect the physical, chemical, mental, and visual processes of our brain. If a patient’s concussion remains undiagnosed and untreated, then their risk for further brain injuries increases, and their ability to do day-to-day activities decreases [8]. Therefore, diagnosing and treating concussions requires a team of diverse health professionals that specialize in the various processes of the brain and body. One of those health professionals is an optometrist, also known as a doctor of optometry. Optometrists and those who specialize in neuro-optometric rehabilitation can provide a necessary treatment for those affected by the visual symptoms of TBI [8,10].
Neuro-optometric rehabilitation is a form of vision therapy that can retrain the brain after injury [10]. This form of therapy is made possible by a property of the brain called neuroplasticity, which refers to the rewiring of neural connections that allows for self-repair. As the brain is recovering, it needs help reprogramming itself to properly process visual input again. The recovery process is largely reliant on neuroplasticity since it is the rewiring of neurons that allows for the restoration of previously damaged cognition. Retraining the brain can be done through the use of treatments such as visual exercises, digital aids, and specialized lenses. There are immediate signs of relief once treatment starts. However, the extent of improvement depends on the cause of the brain injury, the individual’s health, and the commitment to treatment [10].
While the ability of our eyes to be able to see a singular object in front of us is a process we are not necessarily conscious of, it is possible to increase our awareness of this ability [10]. Increasing our awareness will ultimately improve our convergence skills and our brain’s ability to process visual information. One of the treatments an optometrist can give to improve the patient’s convergence skills is a visual exercise similar to Dr. Kawata’s NPC assessment [9]. Instead of using a Snellen chart, a simpler object such as a pencil with a brightly colored eraser can be used [14]. The patient has to be seated or standing tall with their head upright, and holding the pencil in front of their nose. The patient moves the pencil towards their nose slowly while focusing their eyes on the eraser. When the patient begins to experience diplopia (double vision) and blurred vision, they have to stop moving the pencil towards their nose. The presence of the following symptoms of convergence insufficiency mean that the eyes are no longer converging or focusing on the eraser properly. The patient can readjust their eyes by moving the pencil back out away from the nose some distance until the pencil appears as a singular and clear object again. Over time, the patient should be able to bring the pencil very close to their nose without experiencing convergence insufficiency, indicating an improvement of their convergence skills [14].
Alleviating visual symptoms such as convergence insufficiency is just one aspect of concussion recovery. Effective treatment for TBI requires scientific research into how our physical, chemical, mental, and visual processes are affected by concussions. This research has led to various treatments and therapies, such as neuro-optometric rehabilitation. While substantial brain injury research has been conducted on athletes, not everyone who has been affected by brain injury is an athlete.
Traumatic Brain Injury is a Public Health Issue
The American Optometric Association reports that 2.4 million Americans are affected by brain injury each year [15]. The scope of brain injury is larger than just a single activity. TBIs can happen in a variety of different settings. Falls, being hit by or against an object, and motor vehicle crashes were the most common causes of TBI-related emergency department visits at 47.9%, 17.1%, and 13.2%, respectively [16]. Falls and motor vehicle crashes were the most common causes of TBI-related hospitalizations at 52.3% and 20.4%, respectively [16]. Self-harm, falls, motor vehicle crashes were the common causes of TBI-related death at 32.5%, 28.1%, and 18.7%, respectively [16]. 80% of all TBI injuries are reported as concussions [17]. Behind the statistics are people from all different walks of life and backgrounds from children all the way up to the elderly [16]. Being able to put faces to the data can further emphasize the gravity of traumatic brain injury.
A Personal Reflection on Concussion Recovery
Concussions impair the physical, chemical, mental, and visual processes of the brain, but that was something I never truly understood until it happened to me. In 2015, I got my first concussion when a high speed tennis ball hit my face during high school gym class. In 2018, I got my second concussion by hitting my head on a metal corner of a nearby table while fixing a hospital bed. There are a multitude of ways to describe what a concussion feels like from just looking at the medical symptoms and scientific research. However, if I had to describe it from personal experience, I would say that my concussions made me feel like a completely different person for months after each diagnosis. For the longest time, my identity was consumed by my symptoms. While I appeared the same on the outside, I was battling with the pain of my symptoms everyday. Things I had done very easily before my concussions were suddenly very difficult. Going to various treatments and therapies was frustrating at times because I would not always get relief from my symptoms. But without the support of my family, friends, physicians, physical therapists, and an optometrist, I would not be where I am today: talking about my experiences and living a life free of my once overbearing symptoms. Maintaining hope during the recovery process is essential. Through my journey, I learned the true meaning of patience and perseverance, and that is something I am genuinely grateful for.
Millions of people in the US and worldwide are affected by brain injury. A TBI is life-altering, and the people who do survive their TBI have their lives significantly affected for some time. Through researching the health effects of TBI, advancements in the care of such injuries have been made. Specifically, investigation into our oculomotor system has revealed how impactful vision is post-concussion. These discoveries have led to various treatments and therapies, such as neuro-optometric rehabilitation. Access to support and rehabilitation services give those affected by TBI hope that they may experience improvement in their quality of life.
References
Centers for Disease Control and Prevention (CDC). (2019, February 12). What Is a Concussion? Retrieved March 16, 2021, from https://www.cdc.gov/headsup/basics/concussion_whatis.html
Ezell, L. (2013, October 8). Timeline: The NFL’s Concussion Crisis – League of Denial: The NFL’s Concussion Crisis. FRONTLINE. https://www.pbs.org/wgbh/pages/frontline/sports/league-of-denial/timeline-the-nfls-concussion-crisis/
Dewan, M. C., Rattani, A., Gupta, S., Baticulon, R. E., Hung, Y. C., Punchak, M., Agrawal, A., Adeleye, A. O., Shrime, M. G., Rubiano, A. M., Rosenfeld, J. V., & Park, K. B. (2018). Estimating the global incidence of traumatic brain injury. Journal of neurosurgery, 1–18. Advance online publication. https://doi.org/10.3171/2017.10.JNS17352
American Association of Neurological Surgeons. (n.d.). A Neurosurgeon’s Overview of the Brain’s Anatomy. Retrieved March 16, 2021, from https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Anatomy-of-the-Brain
Centers for Disease Control and Prevention (CDC). (2019, February 25). Potential Effects. Retrieved March 16, 2021, from https://www.cdc.gov/traumaticbraininjury/outcomes.html
Centers for Disease Control and Prevention (CDC). (2019, March 11). Symptoms of Traumatic Brain Injury (TBI). Retrieved March 16, 2021, from https://www.cdc.gov/traumaticbraininjury/symptoms.html
Pew, A., & Shapiro, D. (2018, January 18). Football and Brain Injuries: What You Need to Know. National Center for Health Research. https://www.center4research.org/football-brain-injuries-need-know/
American Optometric Association. (2018, August). Concussions, Vision, and Your Eye Doctor. https://www.aoa.org/AOA/Documents/Practice%20Management/Specialties/SPV/AOA-Concussion-FactSheet.pdf
Kawata, K., Tierney, R., Phillips, J., & Jeka, J. J. (2016). Effect of Repetitive Sub-concussive Head Impacts on Ocular Near Point of Convergence. International journal of sports medicine, 37(5), 405–410. https://doi.org/10.1055/s-0035-1569290
Neuro-Optometric rehabilitation. (n.d.). Holistic Vision. Retrieved March 16, 2021, from https://www.holisticvision.com/eye-care-services/neuro-optometric-rehabilitation/
Vimont, C., & McKinney, J. K. (2021, February 25). All About the Eye Chart. American Academy of Ophthalmology. https://www.aao.org/eye-health/tips-prevention/eye-chart-facts-history
American Optometric Association. (n.d.). Visual Acuity. Retrieved March 16, 2021, from https://www.aoa.org/healthy-eyes/vision-and-vision-correction/visual-acuity?sso=y
Mucha, A., Collins M.W., Elbin R.J., Furman J.M., Troutman-Enseki C., DeWolf R.M., Marchetti G., Kontos A.P. (2014). A Brief Vestibular/Ocular Motor Screening (VOMS) assessment to evaluate concussions: preliminary findings. American Journal of Sports Medicine, 42(10), 2479-2486. https://doi.org/10.1177/0363546514543775
Mayo Clinic. (2020, July 16). Convergence insufficiency: Diagnosis and treatment. https://www.mayoclinic.org/diseases-conditions/convergence-insufficiency/diagnosis-treatment/drc-20352739
American Optometric Association. (n.d.). Sports & Performance Vision (SPV). Retrieved March 16, 2021, from https://www.aoa.org/practice/specialties/sports-and-performance-vision?sso=y
Centers for Disease Control and Prevention. (2019). Surveillance Report of Traumatic Brain Injury-related Emergency Department Visits, Hospitalizations, and Deaths—United States, 2014. https://www.cdc.gov/traumaticbraininjury/pdf/TBI-Surveillance-Report-FINAL_508.pdf
Georges, A., & Booker, J. G. (2021). Traumatic Brain Injury. StatsPearls; StatPearls Publishing. Retrieved March 16, 2021, from https://www.ncbi.nlm.nih.gov/books/NBK459300/