A Day in the Life: Living With Charcot Marie Tooth Disease
Author: Pragya Gupta || Scientific Reviewer: Dev Parasania || Lay Reviewer: Markella Vassil || General Editor: Aryan Anand
Artist: Brenna West || Graduate Scientific Reviewer: John Furey
Publication Date: December 18th, 2023
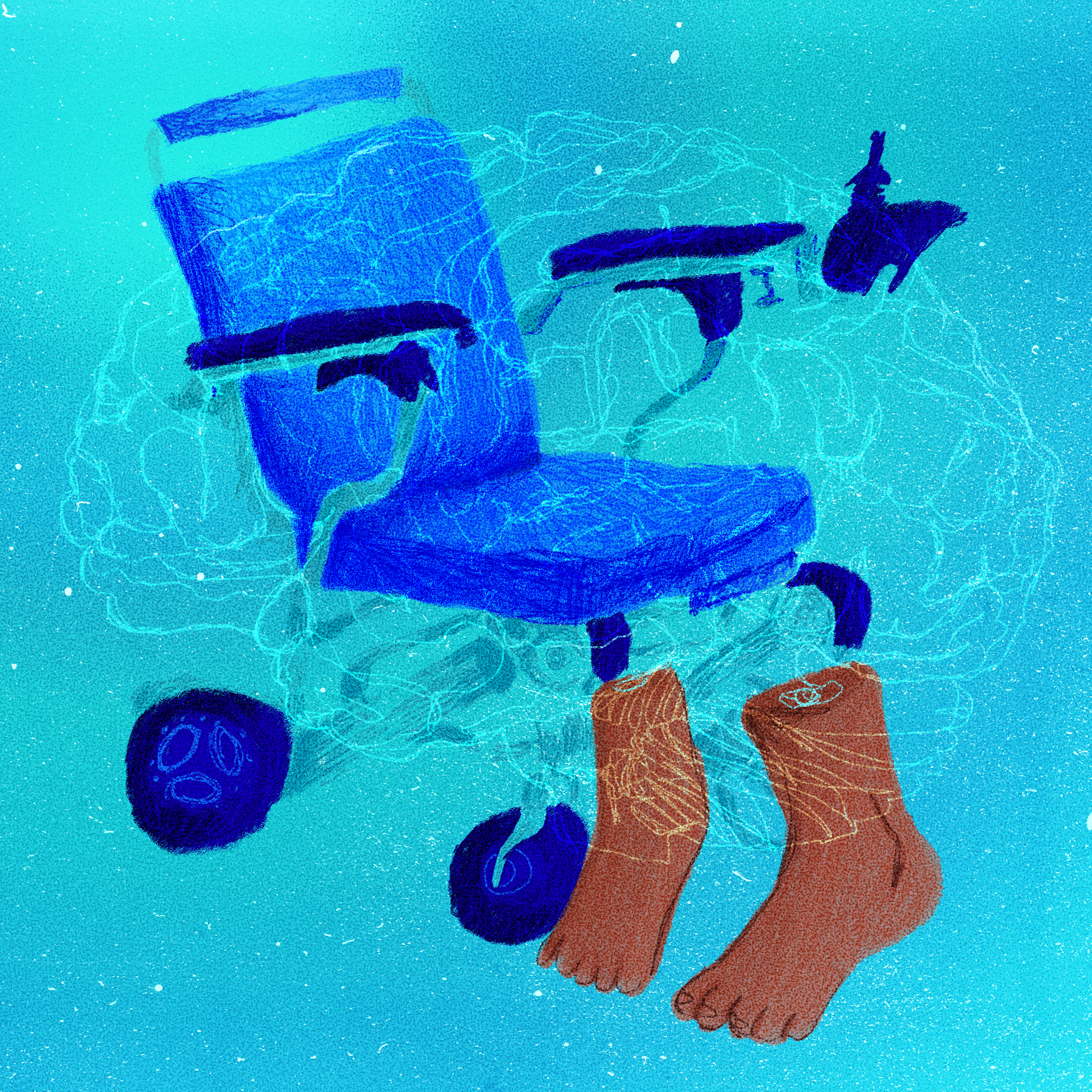
Pragya, Vinnie, wait I need a break, my legs, they feel like jelly, can we stop for a little bit? [1]. As Rai’s compression socks have a limited warranty on their relief, she must stop before she loses all sensation in her feet and cannot walk at all. But it is a daily cycle: she has to walk to and from class, climb up and down the stairs when the elevator does not work, and walk from the distant bus station to her workplace in the city, leaving her with the burden of losing sensation in her limbs. Often, disabilities are very noticeable, but many, though physical in origin, remain hidden from the naked eye. Numerous afflictions are poorly understood, with limited therapeutic techniques that merely provide symptom relief. One such disability, Charcot Marie Tooth Disease (CMT), is a genetic, progressive neuropathy—a disease of the nerves—with a wide range of challenging mental and physical manifestations. Despite advancements in understanding this condition, medical professionals and researchers are still employing various scientific techniques to continue investigating CMT’s origins and the factors contributing to its onset, both on a molecular and environmental level. CMT operates through five main types of neuronal phenomena characterized by their different inheritance patterns; this article investigates the clinical and research implications of the disease, as well as the quality of life for those living with this rare sensorimotor neuropathy.
What is CMT?
Neuropathy, as defined by the National Institute of Health, are nerve-damage disorders. Neuropathy can affect sensory nerves (which provide feeling) or motor nerves (which cause movement), or both, hence sensorimotor neuropathy [2]. CMT, the most prevalent inherited neurological disease, is a progressive sensorimotor neuropathy caused by numerous genetic mutations [3]. Symptoms of CMT include a combination of lower motor neural deficits: weakness in the legs, ankles, and feet, loss of muscle bulk in the legs and feet, high foot arches, decreased ability to run, difficulty lifting your foot at the ankle, decreased sensation in the legs and feet, amongst many more [4]. The severity of CMT varies across its genetic subtypes, but some of its sensory implications include loss of vibration and joint position sense, along with decreased pain and temperature sensation [4]. However, the origins of the physical onsets of this disability lie in deeper, molecular levels, where the hundreds of genes that contribute to the development of sensorimotor functions mutate, leading to CMT.
Inheritance of CMT
Despite its wide variety of physical and sensory onsets, CMT is caused by similar genetic mutations that produce and support the proteins involved in the production of peripheral nervous system myelin sheath [5]. Myelin sheath is an insulating coat, which spans the part of the nerve cell that carries electrical impulses and allows it to be transmitted to the next nerve. This part of the neuron is known as the axon. Myelin sheath allows nerve impulses to travel down the axon quickly and efficiently, and a deficiency of this component leads to the loss of many bodily functions, resulting in disease (such as the more familiar Multiple Sclerosis).
CMT, a hereditary neuropathy, is passed from parent to child in three distinct inheritance patterns: autosomal dominant, autosomal recessive, and X-linked. Autosomal dominant inheritance patterns have the mutated gene on a non-sex chromosome, and one copy of the defective gene is enough to cause CMT [6]. Autosomal recessive patterns are similar; however, two copies of the recessive mutated gene are needed for CMT to be inherited. In comparison, X-linked inheritance patterns involve sex chromosomes, where the mutated gene is present on the X chromosome. In such X-linked neuropathies, one of the two X chromosomes in a female may compensate for the other X chromosome with the defective gene. In contrast, males have one X and one Y chromosome, and the mutated X-linked gene cannot be compensated for. This indicates that X-linked diseases usually affect males more severely than females but cannot be passed from father to son [6]. The three distinct principles by which CMT is inherited can be accredited to the more than 40 genes that have been linked to different subtypes of the disease [5].
Types of CMT and Their Neuronal Mechanisms
The major subtype of CMT is CMT1, which accounts for about 70% of all CMT cases. These cases are caused by a duplication of the PMP22 gene on chromosome 17, an autosomal chromosome [7]. The molecular bases of the PMP22 gene mutation include non-homologous end joining (a pathway responsible for repairing breaks in DNA strands), amino-acid recombination (in which amino acids are switched around, yielding a different protein structure), and replication-based errors [7]. CMT1’s manifestations are slowly progressive; in childhood, abnormalities in myelin sheath structure lead to lower-leg muscle weakness and atrophy (size decrease of a body part), while hand weakness, sensory loss, and foot and leg problems arise later into adulthood [5]. Although CMT is generally inherited through the bloodline, sporadic cases are not completely impossible, as sudden mutations may occur in about 10% of CMT1 [7]. Another type, CMT2, is inherited in an autosomal dominant manner, and its symptoms are similar to those of CMT1 [8]. However, unlike CMT1, it directly affects the axons rather than the myelin sheath [8].
CMTX, the second most common type of CMT, follows an X-linked inheritance pattern, accounting for about 10-15% of all CMT cases. Its physical implications are similar to CMT1 and 2; however, given that it is an X-linked gene, it occurs more commonly in males than females [6]. CMT3 (Dejerine-Sottas syndrome) severely affects the myelin sheath, leading to adverse motor and sensory weakness; CMT4, also a severe type affecting the myelin sheath, begins developing in early childhood, eventually diminishing the ability to walk [9]. As such, there are many other subtypes of CMT, all of which have unique mechanisms both in terms of the mutated gene and their inheritance patterns. However, given that there are so many subdivisions of CMT, it is important to not only learn their mechanisms but also develop an overall understanding of how researchers are working towards providing treatment for those with it.
What Are the Quality-of-Life Implications of CMT?
In Rai’s own words: I was hit hard when I lost my athletic ability due to CMT and could not get a sports scholarship for college — it was something I dreamed of having. On a day-to-day aspect, I have trouble finishing my work and have to account for enough time to leave before and in between classes to make sure I make it on time [1]. People with CMT have shown less strength in both hand grip and tripod pinch (e.g. grip when holding a pencil) than those without [10]. In more extreme cases, according to the members of the CMT Association, some have stiffly curled fingers that hinder their ability to hold and write. Psychological impacts of CMT include irritability, depression, anxiety, feelings of hopelessness, and guilt [11]. A study done on the repercussions of CMT highlights factors such as unemployment and socioeconomic insecurities contributing to increased emotional distress in more severe cases [12]. Given the various mental and physical implications of CMT, it is the responsibility of the non-disabled to accommodate the needs of those with it.
Future of CMT and Developments of Possible Treatments
The future of both the diagnosis and treatment of CMT lies in employing a variety of scientific techniques, such as gene sequencing and gene therapy. Gene sequencing techniques, such as Sanger sequencing (a DNA sequencing method), have been used to identify new genes in CMT families. Next-generation sequencing (NGS) allows the entire genome to be sequenced in a matter of days. Researchers are employing NGS in CMT diagnosis and gene identification which, in turn, has also pinpointed its phenotype [13]. One of the first gene therapies under development involves focusing on reducing the expression of the PMP22 gene to support proper axon myelination. Researchers were able to find that in mice, ascorbic acid, also known as Vitamin C (associated with pro-myelinating effects), was successfully able to suppress the expression of PMP22, leading to improved motor functions [14]. Another approach that scientists are investigating is the amplification of myelin-promoting neural pathways (and inversely downregulating PMP22 formation pathways) through the use of compounds collectively known as PXT3003. In rats, PXT3003 was found to reduce PMP22 formation, again successfully improving axon myelination [14]. Although these experiments have thus far only been successful in mice models, they are promising leads to becoming one step closer to understanding and identifying CMT, allowing for greater support for those living with it. .
Conclusion
There is an overall lack of understanding of rare genetic disabilities along with their implications amongst both the general population and scientific researchers. Charcot Marie Tooth Disease, the most common hereditary sensorimotor neuropathy, was unfamiliar to me until introduced by a close friend living with it. Understanding the genetic basis of CMT inheritance, its types, quality of life implications, and its therapeutic developments has allowed me to gain a greater appreciation for Rai’s determination, strength, and courage. Despite the mental and physical setbacks brought upon by CMT, she is not only a role model for educating her peers about rare diseases, but also a passionate advocate of social and physical accessibility for all disabled persons. In turn, it has inspired me to educate others about rare diseases such as CMT, for which I look forward to seeing greater advancements made in treatments, accommodations, and societal support for those affected.
References
Gupta, P. (personal communication with Rai)
Szigeti, K., & Lupski, J. R. (2009). Charcot-Marie-Tooth disease. European Journal of Human Genetics, 17, 703-710. https://doi.org/10.1038/ejhg.2009.31
https://www.ninds.nih.gov/health-information/disorders/charcot-marie-tooth-disease
https://www.mda.org/disease/charcot-marie-tooth/causes-inheritance
Vallat, J. M., Mathis, S., & Funalot, B. (2013). The various Charcot-Marie-Tooth diseases. Current Opinion in Neurology, 26(5), 473-480. DOI: 10.1097/WCO.0b013e328364c04b
https://charcot-marie-toothnews.com/charcot-marie-tooth-type-2-cmt2/
https://www.nhs.uk/conditions/charcot-marie-tooth-disease/causes/
Mori, L., Schenone, C., Cotellessa, F., Ponzano, M., Aiello, A., Lagostina, M., Massucco, S., Marinelli, L., Grandis, M., Trompetto, C., & Schenone, A. (2022). Quality of life and upper limb disability in Charcot-Marie-Tooth disease: A pilot study. Frontiers in Neurology, 16. https://doi.org/10.3389/fneur.2022.964254
Ivanovic, V., Bjelica, B., Palibrk, A., Brankovic, M., Bozovic, I., Basta, I., Savic, A., Stojanovic, V. R., & Kacar, A. (2022). Physical and Mental Aspects of Quality of Life in Patients with Charcot-Marie-Tooth disease Type 1A. Frontiers in Neurology, 13. doi: 10.3389/fneur.2022.852150
Rossor, A. M., Polke, J. M., Houlden, H., & Reilly, M. M. (2013). Clinical Implications of Genetic Advances in Charcot-Marie Tooth Disease. Nature Reviews Neurology, 9, 562-571. https://doi.org/10.1038/nrneurol.2013.179
Fridman, V., & Saporta, M. A. (2021). Mechanisms and Treatments in Demyelinating CMT. Neurotherapeutics, 18, 2236-2268. https://doi.org/10.1007/s13311-021-01145-z