Walking Dead or Alive? Life with Cotard’s Syndrome
Author: Sarah Bhanushali || Scientific Reviewer: Christopher Mejia-Gonzales || Lay Reviewer: Markella Vassil || General Editor: Jam Stebbins
Artist: Rebecca Mascione || Graduate Scientific Reviewer: Jordan Denaver
Publication Date: December 16th, 2024
CONTENT WARNING: Content in this article discusses mental illnesses, graphic descriptions of death, and related distressing themes. Reader discretion is advised.
Introduction
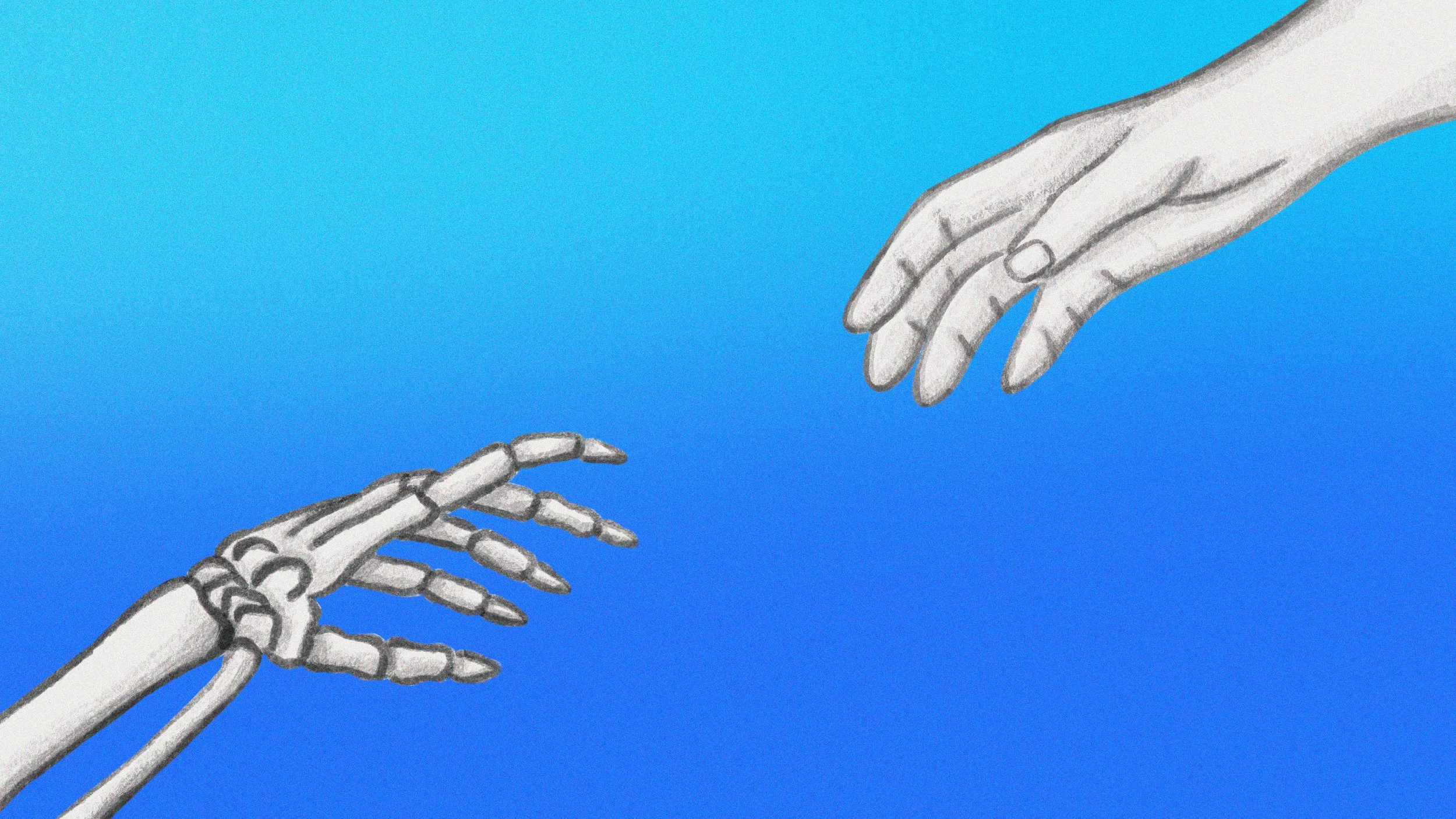
What if you believed your organs had decayed despite moving and interacting with the world? What if you felt you no longer existed or, paradoxically, were immortal? What if, defying all logic, you became convinced that your body was an empty shell? For individuals with Cotard’s syndrome, this unsettling experience is the reality of daily life.
Cotard’s syndrome, also known as walking corpse syndrome, leads to a sense of detachment from one’s identity and a distorted perception of reality [1]. Individuals with this condition also find connecting with the world and those around them challenging. Doctors diagnose Cotard’s syndrome based on two key features: a distorted self-view and the persistence of these distorted beliefs despite clear evidence to the contrary [1].
With only around 200 documented cases worldwide, Cotard’s syndrome remains one of the rarest neuropsychiatric disorders ever recorded [2]. Studying this disorder reveals how the brain perceives reality and what happens when that process is disrupted. Understanding Cotard’s syndrome helps to understand the intricate connection between the brain, identity, and reality perception.
The Case of a Woman’s Journey Through Cotard’s Syndrome
Ms. L had once lived a relatively stable life, but her life changed when she began experiencing intense and unsettling beliefs about her existence. A 53-year-old Filipino woman, Ms. L, was admitted to a psychiatric unit after her family made an emergency call. Convinced she was a corpse, she begged her family to take her to a morgue, insisting that she belonged among the dead. She persistently complained that she smelled like rotting flesh, and she felt haunted by paranoia. When she arrived at the psychiatric unit, she feared that the paramedics were attempting to set her house on fire. In addition to her delusions, she exhibited signs of depression, including hopelessness, minimal appetite, and intense fatigue–a terrifying reality for someone living with Cotard’s syndrome.
Prior to moving to the United States, Ms. L had been prescribed antidepressants, but she could no longer recall their name or dosage. Upon her admission, physicians prescribed her a new regimen of antidepressant medications to help with her symptoms. However, her health worsened with her reluctance to consume food and medication. Her condition left her body in a fragile state, resulting in dangerous electrolyte imbalances, and her neglect of personal hygiene exacerbated her physical condition.
The severity of Ms. L’s decline prompted her family to seek legal action to force treatment. With a revised medication regimen, Ms. L’s condition gradually improved. Over a month, her health significantly improved, and she experienced a remarkable transformation. Ms. L went from pleading to be sent to the morgue to looking forward to her future [3].
Symptoms & Risk Factors
Indicators of Cotard’s syndrome can vary widely but typically involve profound delusions and a severe distortion of reality, often leading to individuals believing that parts of their body, vital organs, or themselves as a person do not exist [1]. These delusions, known as nihilistic delusions, can result in neglect of basic living needs, specifically self-starvation and reduced motor activity, leading to the refusal of food and lack of voluntary physical activity [4]. In rarer cases, individuals may believe they are immortal or become convinced they will never die, which can lead to dangerous behavior, injuries, or death [5]. Alongside these delusions, individuals with Cotard’s syndrome may exhibit signs of suicidal ideation and co-occurring mental health disorders, such as anxiety and depression [5].
Cotard’s syndrome can manifest at almost any age, but it is most common in individuals in their 50s, with a higher prevalence in women [6]. Those with a history of severe depression or other psychiatric disorders are at an increased risk of developing this condition [6].
Research has established a strong link between Cotard’s syndrome and underlying neurological conditions [7]. Neurodegenerative diseases, such as Parkinson’s and Alzheimer’s, can trigger the development of Cotard’s syndrome due to their effects on brain function and perception [7]. Additionally, other neurological issues–such as stroke, subdural hematoma (bleeding outside the brain), multiple sclerosis, migraines, and encephalopathy (where toxins impact brain function)–have also been associated with Cotard’s syndrome [8].
Brain Abnormalities
The exact cause of Cotard’s syndrome remains unknown, but a variety of neurological and biochemical factors contribute to its development. Several brain regions, including the frontal, temporal, and parietal lobes, are integral to perception and identity. Damage or abnormalities in these regions can distort self-perception and lead to delusions that are characteristic of Cotard’s syndrome [9].
For instance, the non-dominant frontal lobe (typically on the brain’s right side) is often affected by cerebral atrophy, a loss of neurons or neuronal connections [10]. This region is essential for body awareness, identity processing, and integrating sensory information. Damage to it may explain the disconnection between reality and one’s sense of self observed in Cotard’s syndrome [11].
Similarly, damage to the parietal lobe–a region responsible for spatial cognition–can result in the neglect of one side of the body, further distorting self-awareness [12]. Lesions in this area can also manifest as a form of neglect, characterized by an inability to accurately perceive and recognize one’s body parts, further distorting self-awareness [12].
Moreover, the dorsolateral prefrontal cortex, located in the frontal lobe, is involved in cognitive control and emotional regulation [13]. Impairments in this area can disrupt brain activity and contribute to nihilistic delusions [14]. Meanwhile, the temporal lobe’s connection to the limbic system is vital for memory and emotional regulation [15]. Damage to the neural circuits linking these regions can result in misunderstandings of identity and distorted sensory processing [5].
In addition to structural damage in specific brain regions, disruptions in cerebral blood flow also contribute to the impairment of brain function, causing delusional symptoms seen in Cotard’s syndrome. Proper blood flow regulation is crucial for delivering oxygen and nutrients necessary for brain function [16]. Studies show that patients with Cotard’s syndrome often experience decreased regional cerebral blood flow in areas such as the parietal lobes and dorsolateral prefrontal cortex [17]. These abnormalities can cause neuronal death from lack of nutrients, disrupting homeostasis in the brain and leading to the development of delusions [18].
Neurotransmitter Imbalances
Delusional symptoms of Cotard’s syndrome are linked to imbalances in neurotransmitters–chemical messengers in the brain that carry signals throughout the body [19]. Two essential neurotransmitters, serotonin and dopamine, regulate mood, appetite, sleep, cognitive abilities, and perception [20]. Low levels of serotonin can lead to emotional blunting, where individuals feel a numbness of emotions, potentially fostering the belief that they are no longer alive [21]. Deficiencies in neurotransmitters such as serotonin, dopamine, and norepinephrine are associated with depression and can ultimately lead to severe psychosocial impairment and delusions of being dead.
A shift in the balance of neurotransmitters can have significant implications for brain function [22]. The hippocampus, a brain region crucial for memory formation and emotional regulation, plays a vital role in maintaining this balance. Both excitatory and inhibitory neurotransmitters are present in the hippocampus, namely glutamate and gamma-aminobutyric acid (GABA). Excitatory neurotransmitters increase the likelihood of a neuron firing an action potential–rapid changes in the voltage across the cell membrane–whereas inhibitory neurotransmitters prevent neurons from firing [23]. Increased excitatory and decreased inhibitory neurotransmitters cause neurons to fire more and increase brain activity. This imbalance of both excitatory and inhibitory can lead to psychotic symptoms, including nihilistic delusions [22].
Treatment Options
Despite the severe and complex symptoms of Cotard’s syndrome, numerous treatments consider it curable. The two main types of treatment methods include therapeutic methods and medications.
Cognitive Behavioral Therapy (CBT), a short-term form of psychotherapy that focuses on helping individuals develop strategies for managing mental health challenges, is a highly recommended form of talk therapy for Cotard’s syndrome patients. CBT focuses on current issues that affect daily life and encourages patients to understand how their thoughts and beliefs influence their behaviors [24]. For patients with Cotard’s syndrome, CBT supports a gradual reconnection to reality and targets delusions. Problem-based sessions help patients identify distorted thinking and improve emotional regulation [24].
Since Cotard’s syndrome frequently occurs alongside other mental health conditions such as depression, anxiety, and schizophrenia, treatments typically focus on managing these coexisting symptoms. Medications that are commonly prescribed to focus on these symptoms include antidepressants, antipsychotics, and anti-anxiety drugs. These medications target underlying mental health issues as they minimize delusional beliefs, stabilize mood, and reduce anxiety levels [25]. For example, selective serotonin reuptake inhibitors (SSRIs), such as citalopram, target low serotonin levels to alleviate anxiety and depressive symptoms. Antipsychotics, such as olanzapine, target dopamine receptors to restore imbalances and reduce psychotic symptoms [26].
Electroconvulsive therapy (ECT) is an alternative treatment when medications and talk therapies prove ineffective. During ECT, small electric currents are passed through the brain to induce a brief, controlled seizure, which results in neurochemical changes. These changes can rewire brain circuits involved in mood regulation, disrupting distorted neural pathways and helping to alleviate symptoms of depression and psychosis [27].
Conclusion
The unique characteristics and rarity of Cotard’s syndrome offer valuable insights into how the brain shapes one’s perception of reality and identity. As a neuropsychiatric disorder characterized by nihilistic delusions, Cotard’s syndrome exemplifies the profound effects of brain dysfunction and abnormalities on an individual’s life.
Real-life cases like Ms. L’s illustrate the devastating and significant impact this disorder has on an individual’s sense of self. However, they also demonstrate the potential for recovery. Despite its complexity, understanding the neurological and psychological factors involved in Cotard’s syndrome enables affected individuals to receive adequate care and treatment. With effective intervention through medications and different therapies, patients can regain a connection with reality and restore their sense of self.
References
Grover, S., Aneja, J., Mahajan, S., & Varma, S. (2014). Cotard's syndrome: Two case reports and a brief review of literature. Journal of Neurosciences in Rural Practice, 5(Suppl 1), S59–S62. https://doi.org/10.4103/0976-3147.145206
Rath, L. (2022, February 13). Cotard’s Syndrome: What Is It? WebMD. https://www.webmd.com/schizophrenia/cotards-syndrome
Ruminjo, A., & Mekinulov, B. (2008). A Case Report of Cotard's Syndrome. Psychiatry (Edgmont (Pa. : Township)), 5(6), 28-29. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2695744/
Merriam-Webster.com Medical Dictionary. (n.d.). Nihilistic delusion. In Merriam-Webster. https://www.merriam-webster.com/medical/nihilistic%20delusion
Bistas, K., & Mirza, M. (2024). Walking corpse syndrome: A case report of Cotard’s syndrome. Cureus, 16(7), e63824. https://doi.org/10.7759/cureus.63824
Moyer, N. (2023, March 9). Cotard Delusion and Walking Corpse Syndrome. Healthline. https://www.healthline.com/health/cotard-delusion
Sahoo, A., & Josephs, K. A. (2018). A neuropsychiatric analysis of the Cotard delusion. The Journal of Neuropsychiatry and Clinical Neurosciences, 30(1), 58–65. https://doi.org/10.1176/appi.neuropsych.17010018
Cleveland Clinic. (2023, October 2). Encephalopathy. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/encephalopathy
Swamy, N. C. K., Sanju, G., & Mathew Jaimon, M. S. (2007). An overview of the neurological correlates of Cotard syndrome. The European Journal of Psychiatry, 21(2), 99-116. https://doi.org/10.4321/S0213-61632007000200002
Cleveland Clinic. (2022, March 10). Brain Atrophy: What It Is, Causes, Symptoms & Treatment. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22515-brain-atrophy
Hoshaw, C. (2021, February 26). Body awareness: How to Deepen your Connection with your Body. Healthline. https://www.healthline.com/health/mind-body/body-awareness
Purves, D., Augustine, G. J., Fitzpatrick, D., Katz, L. C., LaMantia, A.-S., McNamara, J. O., & Williams, S. M. (2001). Lesions of the Parietal Association Cortex: Deficits of Attention. Neuroscience (2nd ed.). Sinauer Associates. https://www.ncbi.nlm.nih.gov/books/NBK10998/
Rilling, J.K., & Sanfey, A.G. (2009). Social Interaction. Encyclopedia of Neuroscience (pp.41-48). Academic Press. https://doi.org/10.1016/B978-008045046-9.01539-4
Arjmand, S., Kohlmeier, K. A., Behzadi, M., Ilaghi, M., Mazhari, S., & Shabani, M. (2020). Looking into a Deluded Brain through a Neuroimaging Lens. The Neuroscientist, 27(1), 73–87. https://doi.org/10.1177/1073858420936172
Filley, C.M. (2002). Neuroanatomy In V.S. Ramachandran (Eds.) Neurosciences and behavioral psychology: Encyclopedia of the human brain (pp.403-422). Academic Press. https://doi.org/10.1016/B0-12-227210-2/00237-5
Gofur, E. M., & Bordoni, B. (2023). Anatomy, Head and Neck: Cerebral Blood Flow. StatPearls[Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK538134/
Nomura, K., Kobayashi, R., Toshinori Shirata, Noto, K., & Suzuki, A. (2024). Longitudinal changes of regional cerebral blood flow on a single-photon emission computed tomography (SPECT) scan in a patient with schizophrenia having Cotard’s syndrome. Cureus, 16(4), e58263. https://doi.org/10.7759/cureus.58263
Hayashi, H., Kobayashi, R., Morioka, D., Saito, Y., Toyoshima, T., & Otani, K. (2021). Improvement of somatic delusions with altered regional cerebral blood flow following electroconvulsive therapy in a patient with schizoaffective disorder. The American Journal of Case Reports, 22, e929800. https://doi.org/10.12659/AJCR.929800
Cleveland Clinic. (2022). Delusional disorder. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/9599-delusional-disorder
Owens, A. (2021, May 7). Serotonin: Affecting Consciousness, Attention, Cognition, and Emotion. HealthCentral. https://www.healthcentral.com/mental-health/serotonin
Ma, H., Cai, M., & Wang, H. (2021). Emotional blunting in patients with major depressive disorder: A brief non-systematic review of current research. Frontiers in Psychiatry, 12, 792960. https://doi.org/10.3389/fpsyt.2021.792960
Selten, M., van Bokhoven, H., & Nadif Kasri, N. (2018). Inhibitory control of the excitatory/inhibitory balance in psychiatric disorders. F1000Research, 7, 23. https://doi.org/10.12688/f1000research.12155.1
Grider, M. H., Jessu, R.,& Kabir, R. (2024). Physiology, Action Potential. StatPearls[Internet].StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK538143/
CAMH. (2018). Cognitive behavioural therapy. CAMH. https://www.camh.ca/en/health-info/mental-illness-and-addiction-index/cognitive-behavioural-therapy
Villines, Z. (2022, June 20). Cotard Delusion and Schizophrenia: Signs and Treatment. MedicalNewsToday. https://www.medicalnewstoday.com/articles/cotard-delusion-schizophrenia#symptoms
Leonard, J. & Ames, H.(2023, December 22). Anxiety medication: List, Types, and Side Effects. Medical News Today. https://www.medicalnewstoday.com/articles/323666#types-of-anxiety-medication
Mayo Clinic. (2018, October 12). Electroconvulsive therapy (ECT). Mayo Clinic https://www.mayoclinic.org/tests-procedures/electroconvulsive-therapy/about/pac-20393894