A Review of Stem Cells in the Treatment of Alzheimer's Disease
Author: Alan Paul || Scientific Reviewer: Mila Janowski || Lay Reviewer: Danny Hoang || General Editor: Shriya Srikoti
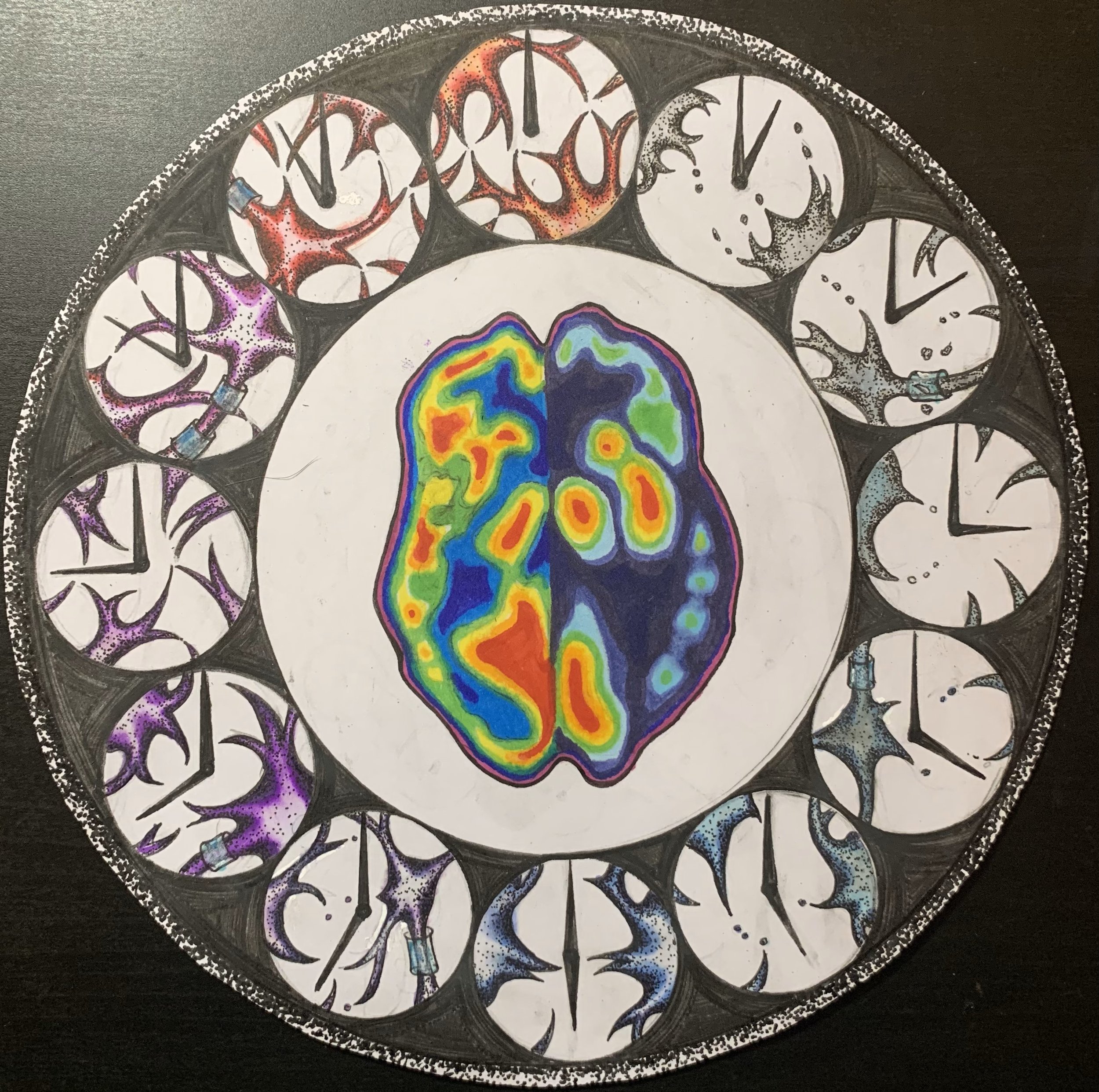
Artist: Willow Tapp || Graduate Scientific Reviewer: Sophia Holmqvist
Publication Date: December 16th, 2024
Introduction
"The transition from being a wife and a love, to a mommy and a caregiver because Leonard developed Alzheimer's - I lost my best friend, my love, my comrade, my business companion, I lost it all. That's the most difficult part [sic]," says Jean [1]. Alzheimer’s disease (AD) currently affects 55 million people worldwide, including Jean and her husband, who must cope with the debilitating effects of the disease daily [2]. Each year, this unforgiving disease claims an additional 10 million diagnoses, demonstrating the growing and devastating impact [2].
AD is characterized by the accumulation of amyloid-beta plaques and tau protein tangles in the brain [3]. These changes result in progressive memory loss, impaired thinking, and behavioral issues, which ultimately affect a person’s ability to perform daily activities [3]. Despite its prevalence, a cure for AD remains elusive. Current treatments may slow disease progression but cannot effectively reverse or prevent its onset. This limitation has sparked an international race among researchers to discover novel therapies that can cure AD instead of slowing progression. Among these, stem cell therapy has emerged as a therapeutic option with increasing promise.
Stem cells have garnered significant attention in medical research due to their ability to differentiate into different cell types and regenerate damaged tissue [4]. They represent a novel approach to combating the underlying causes of AD. However, which types of stem cells hold the most promise, and what mechanisms make them useful? Exploring these mechanisms, their applications, and the challenges associated with their use reveals the transformative potential of stem cell therapy in the fight against AD.
Types of Stem Cells Used
Mesenchymal Stem Cells (MSCs) are cells capable of differentiating into various cell types, including blood vessels, connective tissue, bone cells, lymphatic tissue, and nerve tissue [4]. They are extracted from bone marrow, placentas, umbilical cord blood, and fat obtained via liposuction, a surgery to remove fat from specific body areas [4,5]. MSCs are a highly valuable resource in research due to their unique properties, including their ability to regulate immune cells, decrease inflammation, and signal the regeneration of nearby tissues [6]. Therefore, MSCs are a strong candidate for regenerating neural tissue damaged by AD.
Olfactory Ecto-Mesenchymal Stem Cells (OE-MSCs) are a subgroup of MSCs. The key difference, however, is that OE-MSCs localize to the nasal lamina propria–a region lining the roof and upper section of the septum and the side walls of the nasal cavity [7]. OE-MSCs have similar benefits to regular MSCs, but are predisposed to differentiate into neural cells because they originate from an area densely packed with potent neural stem cells [7].
Human Neural Stem Cells (hNSCs) are derived from fetal brain tissue, embryonic cells, and the cerebellum in adults [8]. Key traits of hNSCs include their ability to slow AD progression and decrease inflammation in neural tissue. This anti-inflammatory effect is primarily due to the secretion of pro-resolving mediators, such as cytokines and growth factors that modulate the immune response [8]. By reducing neuroinflammation, hNSCs foster a more favorable environment for neurogenesis, promoting the development and strengthening of neural tissue. This process may potentially repair damaged brain areas affected by AD [8].
Mechanisms of Action
Stem cells show promise in altering AD progression by either preventing the disease or reversing pre-existing neural damage. Some mechanisms involved in this are direct differentiation into neurons, neurotrophic factor secretion, and reducing oxidative stress [4].
Direct differentiation guides undifferentiated infant stem cells to a specific region of body tissue. Growth hormones and factors then encourage the cells to match the surrounding tissue as they mature. Therefore, it is possible for these undifferentiated stem cells to replace the dead or damaged neurons caused by AD [9]. Scientists have achieved this process using two primary approaches: (1) promoting the stem cells to differentiate into neural tissues after implementation into the body, or (2) pre-differentiating stem cells in a controlled laboratory setting into specific tissue types before reintroducing them to the body [10].
All three stem cells can secrete neurotrophic factors. These are a group of peptides or proteins that support the growth, survival, and differentiation of neurons, leveraging the body’s natural ability to regenerate some forms of neural tissue if the tissue is damaged [3]. However, these factors have drawbacks, such as managing an appropriate concentration, transporting them precisely to locations of damaged or dead neurons, and managing the potential unknown side effects from overstimulating the body’s natural growth and repair systems [3].
Oxidative stress is a chemical process that occurs in the brain when excessive reactive oxygen and nitrogen species or unstable oxygen and nitrogen molecules disrupt the structure and functioning of healthy cells and DNA [11]. Although the brain has natural defense systems to reduce oxidative stress, these systems can become overwhelmed, causing more neural damage. Oxidative stress can cause the unfolding of proteins, nucleic acids, lipids, or fatty compounds, rendering them non-functional, which can contribute to AD progression [11]. Research has demonstrated that MSCs and hNSCs can protect against oxidative stress differently. MSCs directly reduce oxidative stress by secreting non-enzymatic antioxidants, which donate electrons to the reactive oxygen and nitrogen species and neutralize them [6].
In comparison, hNSCs differentiate into neurons and glial cells, including Schwann cells and oligodendrocytes, which can generate the myelin sheaths of neurons to allow for faster signal transmission and regulate the cell’s homeostasis [8]. hNSCs can also develop into a specific type of glial cell called an astrocyte, which can remove certain amino acids that contain reactive nitrogen species and activate enzymatic antioxidants. Furthermore, they can protect the body from reactive species or use redox-pair reactions [8]. In these reactions, one species donates a pair of electrons to the other to regenerate the reduced forms of antioxidants. These diverse protective mechanisms of MSCs and hNSCs against oxidative stress demonstrate their potential to counteract the damaging effects of unstable oxygen and nitrogen species in the brain, which contribute to the progression of Alzheimer’s disease.
Therapeutic Potential
Stem cell therapy can potentially address key mechanisms driving AD, including the accumulation of amyloid-beta plaques and tau tangles. These abnormal protein accumulations in the brain disrupt neuronal function and trigger inflammation that leads to neuronal death and cognitive decline in AD [10]. MSCS, gNSCs, and OE-MSCs have shown the ability to target these features through various mechanisms. The buildup of amyloid-beta plaques disrupts synaptic function and contributes to neuronal death. MSCs can mitigate this by secreting anti-inflammatory cytokines. These small proteins can act as messengers to regulate immune responses, modulate microglia, and act as an immune cell that patrols the brain and clears amyloid deposits [12]. Moreover, hNSCs have the potential to differentiate into neurons, directly replacing those lost due to buildup-induced damage [8]. Stem cells such as hNSCs can secrete neurotrophic factors like Brain-Derived Neurotrophic Factor (BDNF) and Nerve Growth Factor (NGF), which help stabilize and promote the regeneration of existing neurons, preventing tau-induced damage [9]. Neuroinflammation greatly accelerates AD, and MSCs excel at reducing neuroinflammation through secreting factors that inhibit inflammatory cytokines [10]. By reducing inflammation, stem cells can create a more ideal environment for regeneration. Finally, oxidative stress, which is key to the progression of Alzheimer’s, is reduced by stem cells secreting antioxidants that protect neurons from reactive oxygen species [6].
Challenges
Stem cell therapy for AD holds promise but faces scientific challenges. A major concern is immunogenicity, when the body’s immune system recognizes transplanted stem cells as foreign, which reduces their effectiveness or rejects them outright [9]. Another challenge is tumorigenicity – the possibility of stem cells uncontrollably multiplying and forming tumors [10]. Additionally, the regulatory landscape for stem cell therapies requires rigorous clinical trials before they can be approved for widespread use [4]. The ethicality of where some stem cells are acquired, such as embryonic stem cells, sparks moral debates regarding the implications of their use [11]. These hurdles highlight the need for continued research in refining stem cell research to ensure patient safety and address ethical concerns.
The incomplete understanding of Alzheimer’s disease mechanisms presents a significant challenge for developing effective stem cell therapies. The complex factors between genetic, environmental, and lifestyle factors in AD make it difficult to create targeted treatments. Finally, the variation in the study of disease among patients suggests that a personalized approach may be necessary for treatment to be effective.
The Future
In closing, stem cell therapy represents a new frontier in AD treatment, offering hope to those struggling with AD. While new technology may help enhance treatment safety and efficacy, significant challenges remain in bringing these therapies from the lab to the bedside. More research is necessary to refine techniques, tackle the challenges outlined in the previous paragraphs, and effectively incorporate stem cell therapies into existing healthcare frameworks. Further investigation and cooperation amongst various scientific and clinical fields are crucial in overcoming the barriers in place, as this will ultimately allow stem cell therapies to transition from an experimental approach to a reasonable and accessible option for patients impacted by AD.
References
Georges, J., Georges, L. (n.d.). Leonard and Jean Georges: Alzheimer’s Patient Story Cleveland Clinic. my.clevelandclinic.org/patient-stories/61-slowing-the-onset-of-alzheimers.
World Health Organization (WHO). (n.d.). Dementia. World Health Organization. www.who.int/news-room/fact-sheets/detail/dementia#:~:text=Alzheimer%20disease%20is%20the%20most%20common%20form%20and%20may%20contribute,frontal%20lobe%20of%20the%20brain).
Liu, X. Y., Yang, L. P., & Zhao, L. (2020). Stem cell therapy for Alzheimer's disease. World Journal of Stem Cells, 12(8), 787–802. https://doi.org/10.4252/wjsc.v12.i8.787
Zayed, M. A., Sultan, S., Alsaab, H. O., Yousof, S. M., Alrefaei, G. I., Alsubhi, N. H., Alkarim, S., Al Ghamdi, K. S., Bagabir, S. A., Jana, A., Alghamdi, B. S., Atta, H. M., & Ashraf, G. M. (2022). Stem-cell-based therapy: The celestial weapon against neurological disorders. Cells, 11(21), 3476. https://doi.org/10.3390/cells11213476
The Mayo Clinic Staff. (2019, September 19). Liposuction. Mayo Clinic. www.mayoclinic.org/tests-procedures/liposuction/about/pac-20384586.
Oyebode, O. D., & Tulay, P. (2023). Mesenchymal stem cells applications in Alzheimer's Disease. Global Medical Genetics, 10(4), 382–387. https://doi.org/10.1055/s-0043-1777087
Wang, H., & Dwamena, A. (2024). Olfactory ecto-mesenchymal stem cells in modeling and treating Alzheimer's disease. International Journal of Molecular Sciences, 25(15), 8492. https://doi.org/10.3390/ijms25158492
Chen, K. S., Noureldein, M. H., McGinley, L. M., Hayes, J. M., Rigan, D. M., Kwentus, J. F., Mason, S. N., Mendelson, F. E., Savelieff, M. G., & Feldman, E. L. (2023). Human neural stem cells restore spatial memory in a transgenic Alzheimer's
disease mouse model by an immunomodulating mechanism. Frontiers in Aging Neuroscience, 15, 1306004. https://doi.org/10.3389/fnagi.2023.1306004
Bhatti, J. S., Khullar, N., Mishra, J., Kaur, S., Sehrawat, A., Sharma, E., Bhatti, G. K., Selman, A., & Reddy, P. H. (2023). Stem cells in the treatment of Alzheimer's disease - Promises and pitfalls. Biochimica et Biophysica Acta- Molecular Basis Of Disease, 1869(6), 166712. https://doi.org/10.1016/j.bbadis.2023.166712
Elzayat, E. M., Shahien, S. A., El-Sherif, A. A., & Hosney, M. (2023). miRNAs and stem cells as promising diagnostic and therapeutic targets for Alzheimer's Disease. Journal of Alzheimer's Disease, 94(s1), S203–S225. https://doi.org/10.3233/JAD-221298
Altomara, D. (2022, August 3). The Link Between Alzheimer’s, Inflammation, and Oxidative Stress. WebMD. www.webmd.com/alzheimers/alzheimers-inflammation-oxidative-stress.
Lee, C. Y. D., & Landreth, G.E. (2010).The role of microglia in amyloid clearance from the AD Brain. Journal of Neural Transmission, 117, 949-960. https://doi.org/10.1007/s00702-010-0433-4.