The Hidden Risk of Drug-Induced Parkinsonism (DIP) in Common Medications
Author: Tara Kehair || Scientific Reviewer: Sulaiman Sharief || Lay Reviewer: Lillian Hubbard || General Editor: Regan Skudlarek
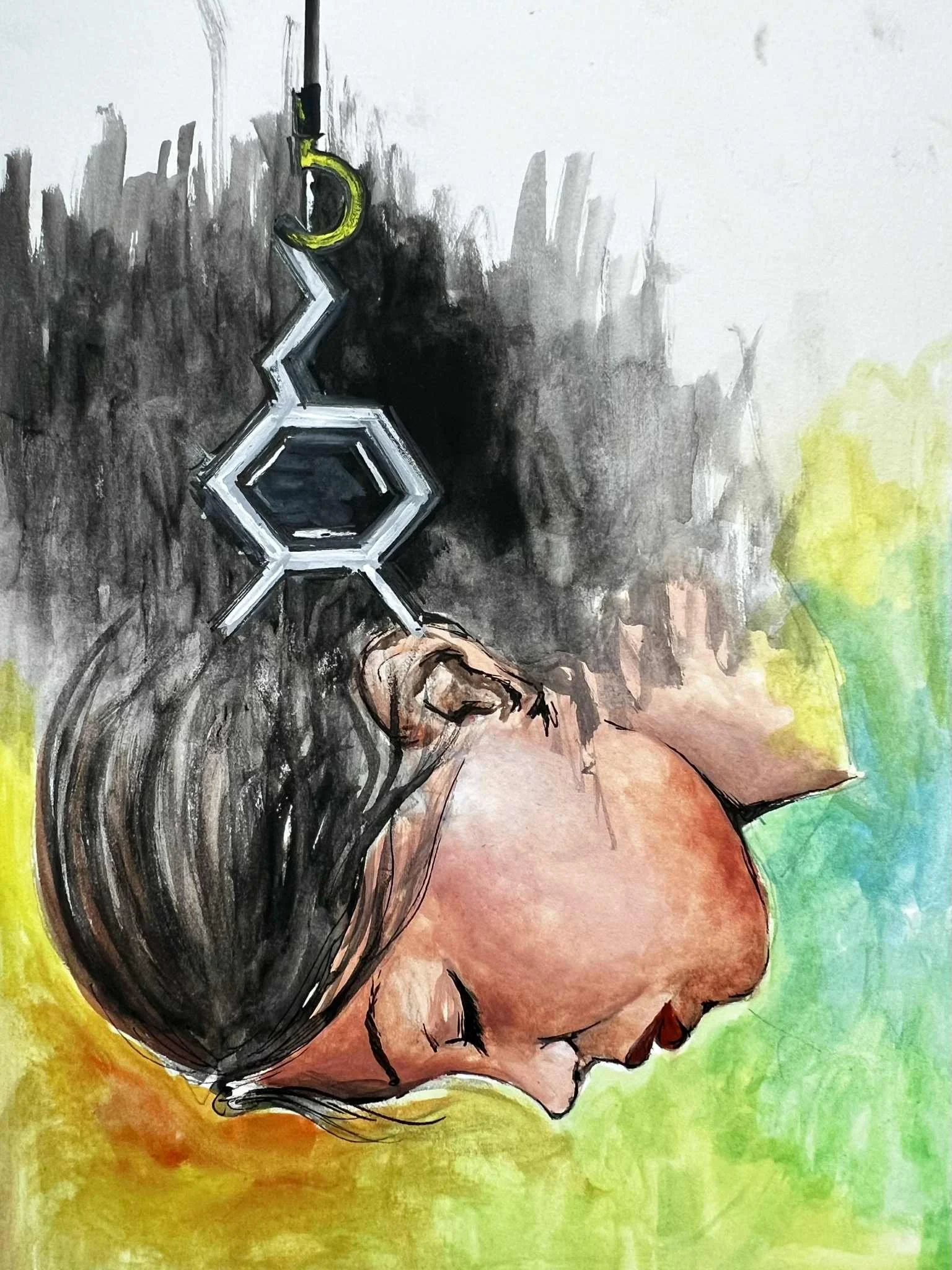
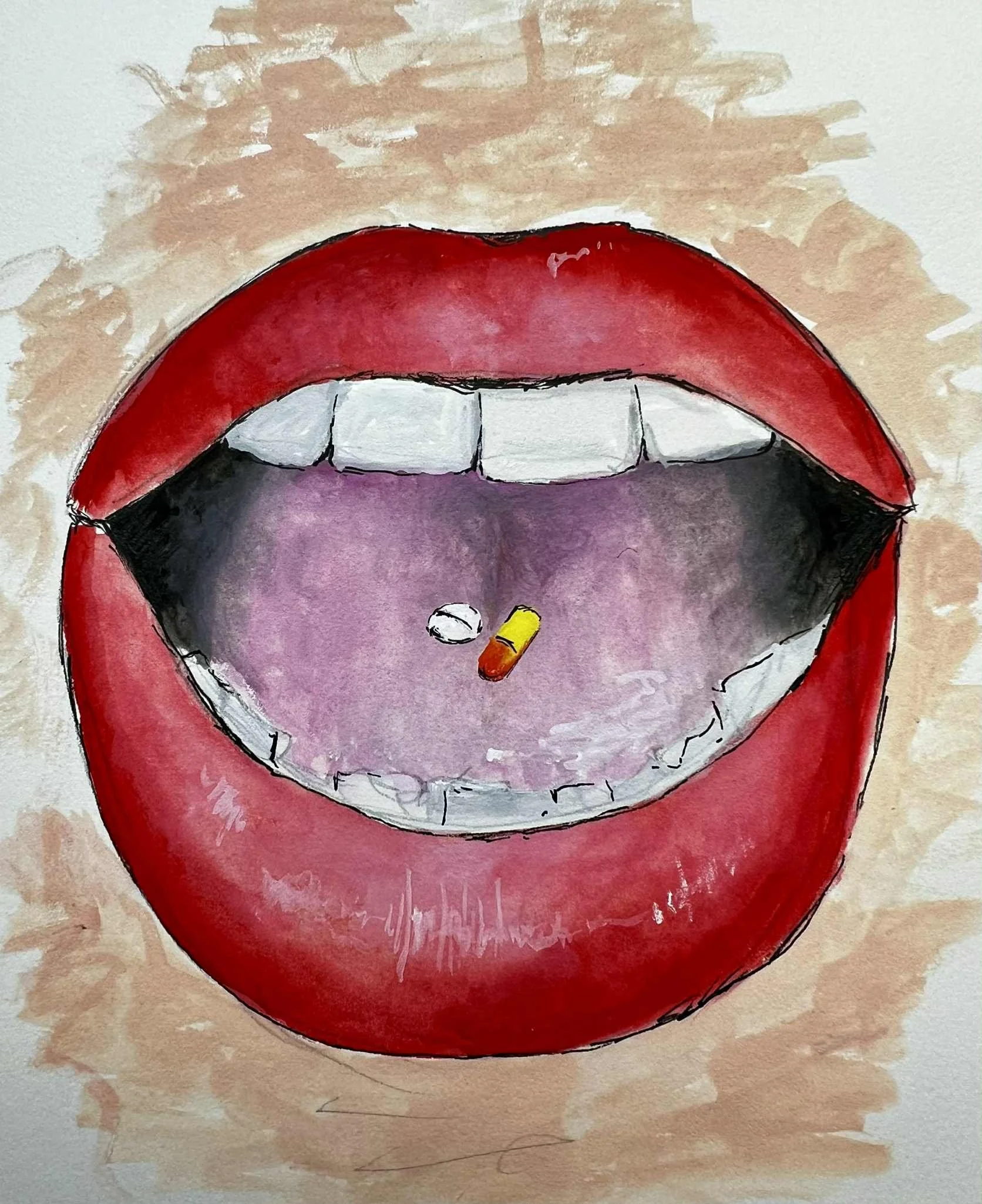
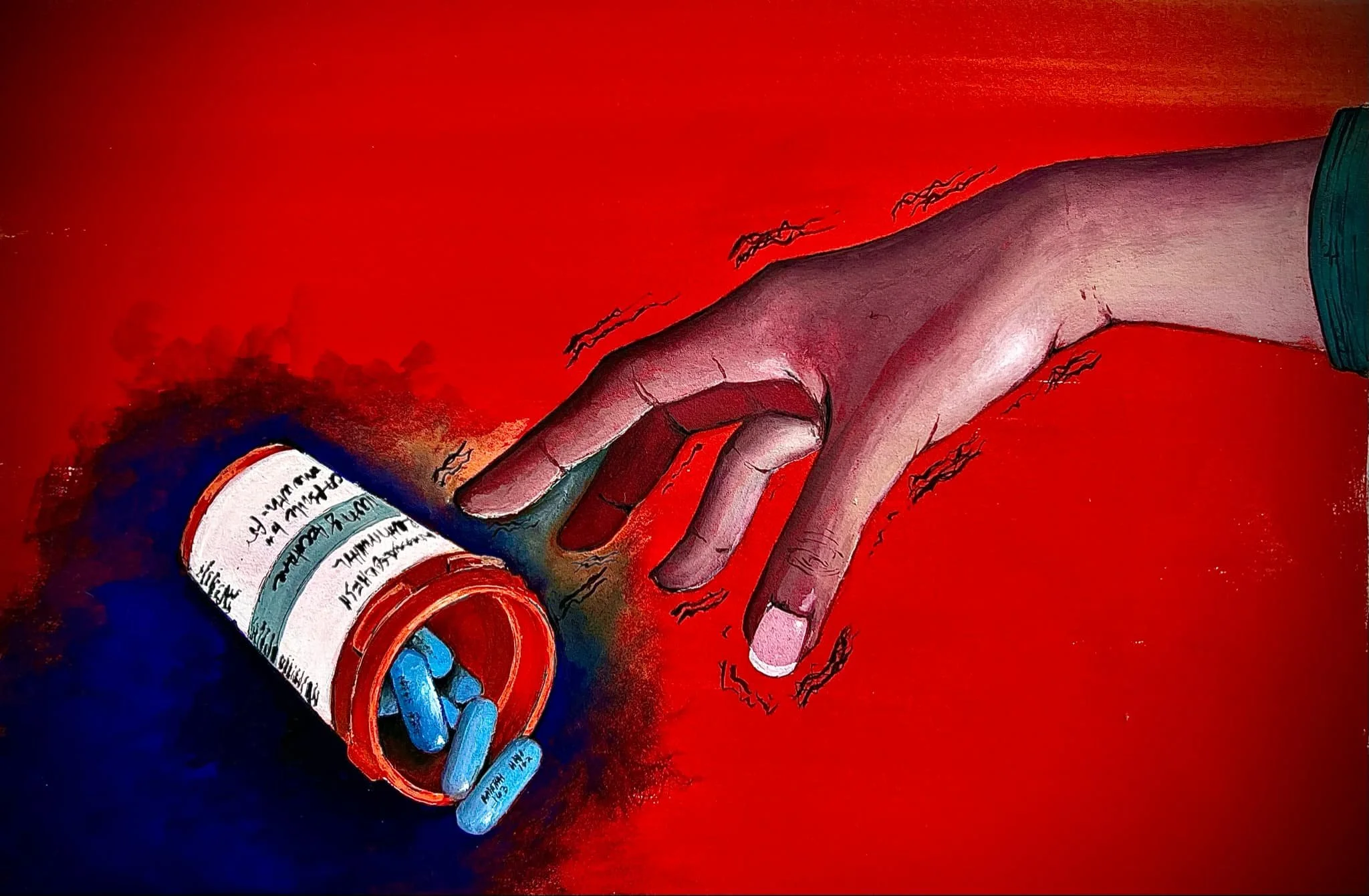
Artist: Reshma Sudhesh || Graduate Scientific Reviewer: Mia Y. Roberts and Syed Farhad Ali Shah
Publication Date: June 11th, 2025
Imagine being prescribed medication to treat a serious condition, only for the treatment itself to induce a disease and leave you with symptoms you never should have had. This situation is a reality for many patients: a cycle of taking medications to treat one condition, just for those same medications to cause another set of symptoms. This phenomena can result in what is known as a prescribing cascade, where a prescribed medication causes an adverse effect that is mistaken for a new condition, leading to a second prescription to treat the adverse side effects. This cycle can continue, resulting in unnecessary medication use [1].
This article will explore the causes of drug-induced parkinsonism (DIP), a condition that occurs through the use of prescription medications or illicit drugs. DIP can cause substantial nervous system symptoms, affecting patients' activities of daily life and causing unnecessary suffering. Yet, like most drug-induced conditions, it is often neglected or misdiagnosed. Exploring the mechanisms of DIP, specifically its causes and symptoms, can help healthcare providers identify and tackle this often overlooked condition. Addressing drug-induced conditions can lead to better health outcomes, prevent unnecessary symptoms, and increase quality of care.
What is Parkinsonism?
Parkinsonism is a broad term used to describe a brain condition that causes symptoms such as tremors, bradykinesia (slowness of movement), and rigidity [2]. It is part of a class of disorders characterized as "neurodegenerative," meaning that neurons in the brain progressively lose function over time [2].
Parkinson’s disease (PD), the most common form of parkinsonism, accounts for 80% of all cases[2]. It is associated with the progressive loss of neurons that release dopamine (DA), a neurotransmitter that plays a vital role in the body’s reward system. Dopamine is associated with feelings of pleasure, learning, memory, and movement regulation [3]. It is produced in the basal ganglia (BG), a part of the brain whose main responsibilities involve motor control and motor initiation [4]. There are two main pathways dopamine follows in this area of the brain: the nigrostriatal, which is involved in motor function, and the mesolimbic, which is involved in motivation and reward function [5]. Damage to cells of the nigrostriatal pathway is associated with PD, causing patients to experience symptoms that affect their balance and voluntary movement [6]. Furthermore, symptoms like difficulty acquiring new skills, anxiety, depression, and other mood disorders can also occur, as the neurons in the BG contribute to procedural learning and emotional processing [7]. Moreover, patients with PD are also at risk of symptoms such as sleep dysfunction, drooling, and even loss of smell [8]. There is no known cause of Parkinson’s disease, which is why it is often referred to as idiopathic Parkinson’s disease. In fact, about 90% of PD cases are idiopathic and only 10% are linked to genetic causes [8].
The second most prevalent type of parkinsonism is drug-induced parkinsonism (DIP) [9]. Unlike Parkinson’s disease, DIP is not idiopathic and has a known cause that is linked to the use of certain medications or illicit drugs. The symptoms of DIP are very similar to that of Parkinson’s disease. However, the way the symptoms manifest and develop differ between the two conditions. Patients with Parkinson’s disease often experience asymmetric or unilateral symptoms that impact one side of the brain and subsequently only one side of the body. These symptoms slowly progress over time and may become bilateral as the disease develops. In contrast, DIP patients often experience symptoms symmetrically and quickly, with little change overtime. In fact, in a study of 190 patients who developed DIP by using antipsychotics, only 20.3% were found to have unilateral movement symptoms, whereas a majority of PD patients experience onset of symptoms on only one side of the body [10].
Further, the symptoms of DIP are often temporary, resolving weeks to months after terminating use of the offending drug. In fact, only 10-50% of patients with DIP experience symptoms that persist or progress after ending drug use [10]. Comparatively, symptoms of Parkinson's disease are permanent. In a study of 136 patients with Parkinson's disease, 75% had worsening symptoms throughout their life with their condition developing into dementia at some point after their diagnosis [11].
What Drugs are Associated with DIP?
Similar to Parkinson’s disease, DIP is associated with low levels of dopamine. However, this deficiency is due to medication usage, rather than a typically unknown cause as in Parkinson’s disease [9]. Prescription medications such as antipsychotics, antidepressants, and calcium channel blockers have all been shown to induce parkinsonism [9]. Similarly, use of heroin has also been explored as a cause of DIP [16], and use of cocaine has been shown as a risk factor for Parkinson’s disease [18]. Each drug category has a different mechanism of interfering with the dopamine pathway and its production in the brain.
First-generation antipsychotic medications, such as haloperidol and trifluoperazine, are used to treat conditions such as schizophrenia and bipolar disorder, both of which are associated with symptoms of psychosis, including hallucinations, delusions, and/or disordered behaviors [12]. Research suggests that schizophrenia and bipolar disorder are linked to increased dopamine signaling in the brain, particularly within the limbic system [13]. The limbic system regulates emotions and behavior, so hyperactivity in this area of the brain leads to the hallmark symptoms of hallucinations and delusions that a patient experiences during psychosis [14]. Antipsychotics aim to treat such symptoms by decreasing levels of dopamine transmission by acting as a competitive inhibitor. Once in the brain, these medications bind to dopamine receptors, preventing dopamine from associating with its receptor and obstructing signaling between neurons [12]. While these medications have been very effective at treating psychotic conditions and decreasing dopamine activity in the limbic system, there remains strong evidence demonstrating their risk for causing parkinsonism, due to their ability to substantially decrease dopamine in the nigrostriatal pathway [13].
Antidepressants, specifically selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), have also been implicated in parkinsonism, and have been found to cause movement issues due to their interference with dopamine [15]. SSRIs are used to treat patients with depression by decreasing reuptake of serotonin in the synapse, leading to increased concentration of serotonin and more activation of serotonin receptors called 5-HT [16]. 5-HT receptors have an inhibitory effect on DA receptors, specifically decreasing the firing rates of dopaminergic neurons in the mesolimbic pathway–the main dopamine circuit within the limbic system [16]. Damage to this pathway, or decreased activity, may contribute to parkinsonism symptoms related to mood and executive function, as motor related symptoms are generally associated with the nigrostriatal pathway of dopamine. Moreover, a review of case reports of SSRI-induced movement disorders found that 14% had parkinsonism-like symptoms [17].
Calcium channel blockers (CCB), a type of medication used to treat heart diseases like high blood pressure or arrhythmias, are also correlated with DIP. They have been shown to reduce dopamine transmission, yet further research is needed to fully understand the mechanistic effects CCBs have on dopamine synthesis, release, and receptor activity [18]. In addition, symptoms do generally improve after discontinuation of the CCB as expected. However, a study of 36 patients with CCB-induced Parkinson’s found that 92% still had a tremor 24 months after CCB withdrawal [19].
Lastly, illicit drug use has been linked to DIP, specifically heroin and cocaine. A case series of seven adults in 1982 found that a certain synthetic heroin strain resulted in irreversible parkinsonism. This heroin was contaminated with 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP), a neurotoxin that targets the dopamine pathway [20]. After entering the blood, MPTP can easily diffuse into the brain as it passes through the blood brain barrier (BBB), the protective semipermeable membrane that lines the brain [21]. Once passing the BBB, MPTP is then converted to its more toxic form, 1-methyl-4-phenylpyridinium (MPP+) ion. This ion can destroy the nigrostriatal pathway, affecting dopamine transmission and mimicking symptoms of PD [21]. Thus, while heroin was the substance used, it was actually the MPTP contamination that led to drug-induced parkinsonism, emphasizing the contamination risks of illicit drug use [20].
Moreover, one study found that cocaine–a stimulant drug–was shown to make cells of the substantia nigra, a part of the BG, specifically more susceptible to MPTP toxicity [22]. This study involved four test groups of adult and in utero mice: control, MPTP exposed, cocaine exposed, and cocaine and MPTP exposed [22]. When exposed to both cocaine and MPTP it was found that both adult and in utero mice were more vulnerable to MPTP toxicity. In comparison, the control group, cocaine exposed, and MPTP exposed groups had no significant changes histologically [22]. This indicates that cocaine use increased the effect of MPTP, suggesting synergistic toxicity between cocaine and MPTP (toxicity induced through interaction between multiple causes) [22]. This is important because it highlights how cocaine may be a potential risk factor for the development of parkinsonism, especially when interacted with a neurotoxin like MPTP [22]. There is no research demonstrating that cocaine can “cause” parkinsonism, which is why it cannot be referred to as a DIP-related drug. However, these findings do show that cocaine users may have an increased risk of developing parkinsonism in the future.
Conclusion
Drug-induced parkinsonism is a serious yet often misdiagnosed neurological condition. The overlap of symptoms that DIP has with PD, as well as risk of prescribing cascades in older adults, makes this condition overlooked. Being aware of what medications are linked to DIP and recognizing the condition early can prevent unnecessary suffering and allow for more accurate diagnoses, patient-centered treatment, and informed prescribing.
Future studies should explore what factors increase an individual's risk of developing DIP. Specific areas for future research include if genetic or environmental factors are associated with DIP or if certain demographics are more at risk. Establishing clinical screening tools for DIP during routine follow-ups, especially for high-risk medications, would be useful in early diagnosis of the condition. In addition, it would be valuable to explore if these drug-induced dopamine impacts do have long-term consequences and if they potentially link to PD. Moreover, research must be conducted to further understand the relationship of illicit drug use and parkinsonism, particularly those involved in the dopamine pathway (such as cocaine, methamphetamine, and heroin). Ultimately, recognizing the reversible nature of DIP underscores the importance of caution healthcare professionals should take in their prescribing practices and the need for continued investigation into neuropharmacological side effects.
References
Mohammad, A. K., Hugtenburg, J. G., Vanhommerig, J. W., van den Bemt, P. M. L. A., Denig, P., & Karapinar-Carkıt, F. (2024). Identifying and quantifying potentially problematic prescribing cascades in clinical practice: A mixed-methods study, Journal of the American Geriatrics Society, 72(12), 3681–3694. https://doi.org/10.1111/jgs.19191
Shrimanker, I., Tadi, P., & Sánchez-Manso, J. C. (2022a). Parkinsonism. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK542224/
Juárez Olguín, H., Calderón Guzmán, D., Hernández García, E., & Barragán Mejía, G. (2015). The role of dopamine and its dysfunction as a consequence of oxidative stress. Oxidative Medicine and Cellular Longevity, 2016(1), 1–13. https://doi.org/10.1155/2016/9730467
Young, C. B., Sonne, J., & Reddy, V. (2023, July 24). Neuroanatomy, Basal Ganglia. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK537141/
Wise, R. A. (2009). Roles for nigrostriatal—not just mesocorticolimbic—dopamine in reward and addiction. Trends in Neurosciences, 32(10), 517–524. https://doi.org/10.1016/j.tins.2009.06.004
Caminiti, S. P., Presotto, L., Baroncini, D., Garibotto, V., Moresco, R. M., Gianolli, L., Volonté, M. A., Antonini, A., & Perani, D. (2017). Axonal damage and loss of connectivity in nigrostriatal and mesolimbic dopamine pathways in early Parkinson’s disease. NeuroImage: Clinical, 14, 734–740. https://doi.org/10.1016/j.nicl.2017.03.011
Tan, L. C. S. (2012). Mood disorders in Parkinson’s disease. Parkinsonism & Related Disorders, 18, S74–S76. https://doi.org/10.1016/s1353-8020(11)70024-4
Zafar, S., & Yaddanapudi, S. S. (2023, August 7). Parkinson Disease. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK470193/
Shin, H.-W., & Chung, S. J. (2012). Drug-Induced Parkinsonism. Journal of Clinical Neurology, 8(1), 15. https://doi.org/10.3988/jcn.2012.8.1.15
Pieters, L. E., Bakker, P. R., & van Harten, P. N. (2018). Asymmetric drug-induced parkinsonism and psychopathology: A prospective naturalistic study in long-stay psychiatric patients, Frontiers in Psychiatry, 9, 18. https://doi.org/10.3389/fpsyt.2018.00018
Aarsland, D., & Kurz, M. W. (2010). The Epidemiology of Dementia Associated with Parkinson’s Disease, Brain Pathology, 20(3), 633–639. https://doi.org/10.1111/j.1750-3639.2009.00369.x
Chokhawala, K., & Stevens, L. (2023). Antipsychotic medications, National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK519503/
Brisch, R., Saniotis, A., Wolf, R., Bielau, H., Bernstein, H.-G., Steiner, J., Bogerts, B., Braun, A. K., Jankowski, Z., Kumaritlake, J., Henneberg, M., & Gos, T. (2014). The role of dopamine in schizophrenia from a neurobiological and evolutionary perspective: Old fashioned, but still in vogue, Frontiers in Psychiatry, 5(47). https://doi.org/10.3389/fpsyt.2014.00047
Chaudhury, S., Kumar, S., & Soren, S. (2009). Hallucinations: Etiology and clinical implications, Industrial Psychiatry Journal, 18(2), 119. https://doi.org/10.4103/0972-6748.62273
Visco, D. B., Manhães-de-Castro, R., Chaves, W. F., Lacerda, D. C., Pereira, S. da C., Ferraz-Pereira, K. N., & Toscano, A. E. (2018). Selective serotonin reuptake inhibitors affect structure, function and metabolism of skeletal muscle: A systematic review, Pharmacological Research, 136, 194–204. https://doi.org/10.1016/j.phrs.2018.09.004
Di Mascio, M., Di Giovanni, G., Di Matteo, V., Prisco, S., & Esposito, E. (1998). Selective serotonin reuptake inhibitors reduce the spontaneous activity of dopaminergic neurons in the ventral tegmental area, Brain Research Bulletin, 46(6), 547–554. https://doi.org/10.1016/s0361-9230(98)00054-9
Dixit, S. (2015). A Case of SSRI Induced Irreversible Parkinsonism, Journal of Clinical and Diagnostic Research. https://doi.org/10.7860/jcdr/2015/11394.5583
Mena, M. A., Garcia de Yébenes, M. J., Tabernero, C., Casarejos, M. J., Pardo, B., & de Yébenes, J. G. (1995). Effects of calcium antagonists on the dopamine system, Clinical Neuropharmacology, 18(5), 410–426. https://doi.org/10.1097/00002826-199510000-00004
Garcı́a-RuizP. J., Javier Jiménez-Jiménez, F., & Garcı́a de YébenesJ. (1999). Calcium channel blocker-induced parkinsonism: clinical features and comparisons with Parkinson’s disease, Parkinsonism & Related Disorders, 4(4), 211–214. https://doi.org/10.1016/S1353-8020(98)00032-7
Nonnekes, J., Post, B., Tetrud, J. W., Langston, J. W., & Bloem, B. R. (2018). MPTP-induced parkinsonism: an historical case series, The Lancet Neurology, 17(4), 300–301. https://doi.org/10.1016/s1474-4422(18)30072-3
Meredith, G. E., & Rademacher, D. J. (2011). MPTP Mouse Models of Parkinson’s Disease: An Update, Journal of Parkinson’s Disease, 1(1), 19–33. https://doi.org/10.3233/jpd-2011-11023
Lloyd, S. A., Faherty, C. J., & Smeyne, R. J. (2006). Adult and in utero exposure to cocaine alters sensitivity to the parkinsonian toxin 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine. Neuroscience, 137(3), 905–913. https://doi.org/10.1016/j.neuroscience.2005.09.035